I’ve been seeing patients in-person since I got vaccinated in January of 2021. Since then I’ve devised and revised my COVID-19 safety procedures more times than I can count. Here’s how they look right now:
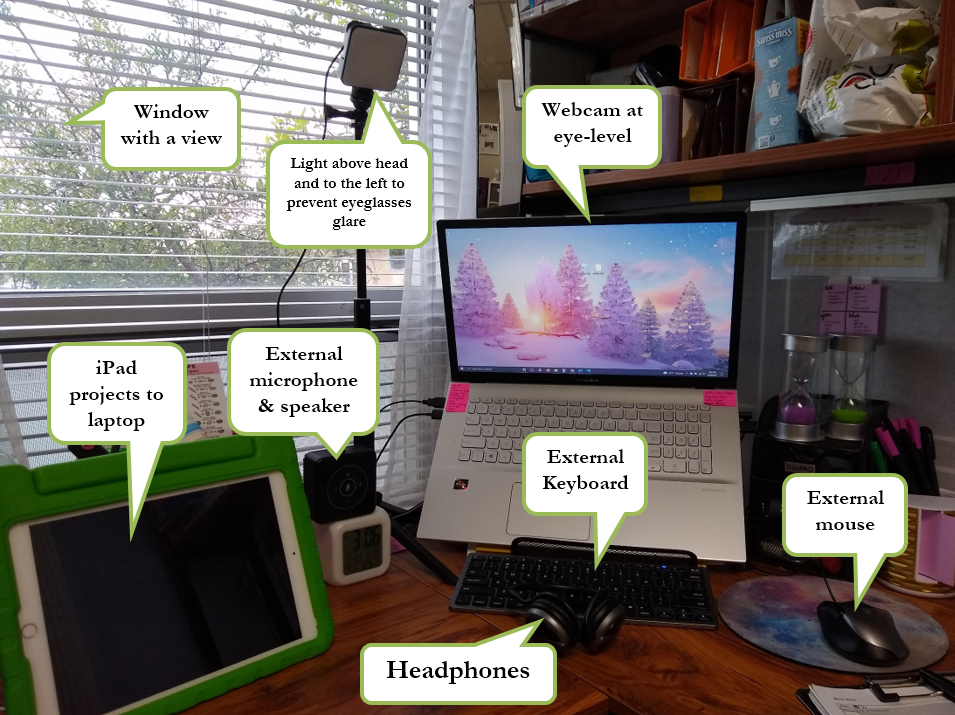
- I’m still seeing 60% of my patients online. That means I only have the germs of 10 patients (plus their parents and myself) cycling through my treatment room. It also means that in the case I need to quarantine it will change nothing for the treatment of most of my patients. For test best telehealth appointments I do the following…
- I use an external microphone so my patients can hear me more clearly.
- I use headphones so I can hear the patients more clearly. Despite them, it’s still often difficult to hear their production of /s/ so I target /z/ instead. My one patient who was voicing /s/ is in-person so I can hear how she’s doing.
- I positioned my computer desk in front of a window so I can do the 20/20/20 rule my optometrist gave me for my “Zoom eye problems.” With this rule I try to look at something 20 feet away for 20 seconds every 20 minutes that I’m on the computer. Since my appointments are 45-minutes each I only do it half as often as I should. I’ve also formed the habit of taking care of things around the office between appointments to give my eyes a rest. These measures, combined with my blue-light-filtering lenses have helped my eyes a ton!
- I keep hand sanitize on my desk and use it often, despite the fact that 99.95% of COVID-19 infections are transmitted through the air (so only .05% of them are from fomite transmission, which is transmission from surfaces).
- I only use paper for my data sheets and test protocols – otherwise everything is digital. I can’t get away from using paper data because I often change what I do during an appointment based on how a patient did last week and I use my data sheets to plan for future appointments, too.
- Now that I have an official desk and office chair in my treatment room I needed a way to close it in and protect little fingers from it – so I bought privacy panels, which also help for kids who are more easily distracted.
- All iPads, thermometers, tables, chairs, knobs, and switches are disinfected between patients.
- All toys are also disinfected between patients. I’ve turned one of my fabric cube storage bins into the “dirty toys bin” and that’s where I put the toys after they’re touched.
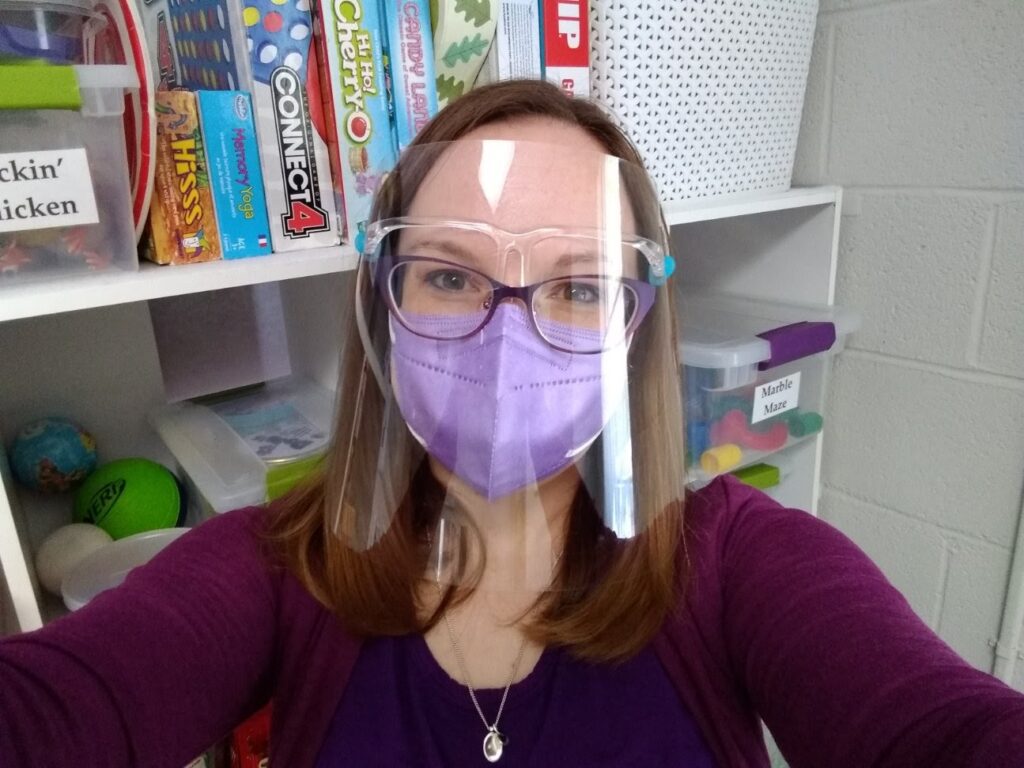
- I wear a KN95 mask and face shield during my in-person appointments. Here’s my post about which PPE I’m using with patients, depending on their treatment.

- What will be the parent-corner is currently where I’m sitting for socially-distanced treatment. I’ve added a “disinfection station” to this area. On it I have…
- …my thermometer.
- …Caviwipes & gloves for using them.
- …my face shield.
- …rubbing alcohol in a spray-bottle to use on face shields between close-contact patients are too cognitively young to wear masks or face shields.
- …rubbing alcohol pads, which I sometimes need to get the little fingerprints off my face shield.
- …masks for parents who forget to wear them into the treatment room.
- …recyclable child-size KN-95 respirator masks for me and the patients whose parents requested them.
- …Cavicide, back-up Caviwipes, back-up hand sanitizer, and back-up face shields.
- I have 3 feet of distance (which is what’s recommended for younger children) taped out between my spot and the kids’/parents’ part of the room.

- For the kids’ spot…
- …I keep the kids’ chairs pulled out so they don’t have to touch them if they don’t want to.
- …I keep a bottle of hand sanitizer on the table.
- …I have a “speech mirror” that they can easily turn to look at while they’re moving their tongues, jaws, and lips to be able to produce speech sounds correctly. Once I’m able to be in closer contact with the kids we’ll be able use this mirror to look at each other as we’re working on our speech sounds and that will make our speech droplets land on the mirror, instead of each others’ faces!
- …I have my “Zones of Regulation” poster with an extra printed check-in/plan. This will help kids maintain optimal regulation even if they’re feeling nervous about re-opening.
- I’m disinfecting my floor between patients. This is because…
- …I have patients who are completely or just cognitively young enough to eat things off of the floor.
- …I have a lot of patients who work best when they’re able to sit on the floor. I know Occupational Therapists have information about core muscles and proprioception that explain this.
- …I have patients who struggle with saliva management so I often have drops of saliva on my floor.
- …when we cough, sneeze, or speak the droplets we don’t catch in our masks or elbows fall to surfaces such as tables and the floor.
- I bought a bubble machine so my germs are not in the bubbles. I haven’t seen any research on bubble-transmission, but I’d rather be safe than sorry.
- I’ve placed the toy shelves into the 3-foot distance zone to protect them from hands. I’ve also added shelf covers which protect them from hands, air droplets, and the bubble solution. An added bonus is that they help kids who are more easily distracted, too!
- Many of my in-person patients have their own shelf with their face shield, individual toys, and individual treatment supplies such as kinetic sand to provide sensory supports and/or suckers to push their tongues back for /r/. These are disinfected and/or replaced monthly.